I’ve always wanted to be a father, or at least to teach a child to read, ride bikes and tell stories. For me it was less about transmitting genes, and more about the lived experiences you can share with a new generation. I clearly recall the joy of babysitting when I was a young man. After I got my drivers license I would drive my parent’s 1989 Grey Oldsmobile Cutlass Supreme piled high with neighborhood kids to McDonalds for a meal (I know, not great, but their product is addictive and this was the 90s). After everyone ate, I’d supervise the kids as they played on the plastic and steel play equipment.
Filled with pride for delivering joy to these kids, I thought, “This is what parenting must feel like?”
Fast forward a few decades, I became a dog father to Luna and Maple, and while those were my fur babies, they were not my real ones. Luckily, Emily and I had a plan.
Our first home in Tacoma, WA
Shortly into our relationship, Emily shared that she is a carrier for a genetic condition that causes Fragile X Syndrome, causing cognitive developmental delays and other health conditions for those affected. For carriers—almost exclusively females—the condition doesn’t show physically or cognitively, but can accelerate the onset of menopause from a more typical mid-50s to early 40s or even late 30s. Other reproductive issues can arise as well, including decreased ovulation and fertility.
“We’ll figure it out”, I offered convincingly.
While I didn’t know much about the condition, I had unfounded confidence that we would find a way. First of course, we needed to date a bit more and build a shared vision of our future together. Over the next year we did just that—traveling internationally, running trail races throughout the Pacific Northwest, moving in together and buying a home in the 6th Ave neighborhood of Tacoma. The broad-leafed Maple that towered over the backyard meant we were home. We were building something beautiful!
Making a Family
After a year in our home, Emily and I decided we were ready to start our first “round” of IVF, or in vitro fertilization and genetic testing. While we had yet to wed, we both knew the biological clock is ticking (I always hear this phrase spoken as Marissa Tomei’s role in My Cousin Vinny). The first part of this physically and financially grueling experience involves going into Seattle Reproductive Medicine and having a genetic model made from blood taken from Emily and myself. Armed with this information, the embryos we created could later be tested to screen for genetic abnormalities.
Our next step involved Emily taking weeks of daily injections to cause hyperovulation while timing things with her normal menstrual cycle plus going into SRM for a few ultrasounds to count the number of embryos that were maturing. The more we could harvest at once the better as this gave us a better chance of creating an healthy embryo.
The day before “go” day, Emily administered a different (and giant) “trigger” injection. The next morning we went into SRM and with Emily under sedation the embryos were removed by Dr. Dudley in a quick, but nerve-racking procedure. After Emily recovered, I walked her down to the car. She slept in the passenger seat as I parked in the loading zone of the South Lake Union Whole Foods to buy grilled paninis. I then jumped back into the car and directed it south.
Let’s go home.
The “trigger” injections were no joke. Emily had lots of injections over months, but the triggers were the biggest trouble.
While running the first cycle of IVF, we also emigrated eggs Emily had previously had harvested and frozen years earlier while working as a pilot in Canada. After they made it through the border, the eggs were fertilized with my sperm along with the eggs that were just harvested in the first cycle. Next they were gestated for five days in a petri dish. The gestation period is so the young embryo could divide. Doctors could pluck a few cells from the outside of the blastocyst. These cells were then sent for genetic testing. The results would then be compared against the genetic model Emily and I had created a few months earlier to assess health and viability.
A Game of Fractions
The experience of IVF is all about fractions. The goal is to get a big numerator. Why is this crucial? Because at each stage in the process your viable embryo count gets reduced lower and lower. You might start with 10 eggs from a cycle, but only six fertilize. Of those six, four may turn out to be genetically abnormal, and then only two survive being thawed for implantation. And that’s all just for the chance for the young embryo to take once it is implanted into the womb. It is not uncommon for early miscarriages to occur for IVF and non-IVF pregnancies as well—happening as frequently as 10 - 20% of all pregnancies according to some studies.
Going into the first round we knew we had to be financially prepared to do at least a second round of IVF (plus use the eggs that we brought back from the one egg harvest Emily had in Canada) as we likely wouldn’t get enough eggs from the first round we just completed in June. So, July came around and it was Groundhog Day again: injections, trigger shot, harvesting the eggs, insemination, gestation and then testing. While the process was not as all encompassing as pregnancy, the egg maturation period Emily endured was far from nothing. The drugs she took caused her ovaries to swell. She also couldn’t live her normally active lifestyle as a runner because there was fear that excessive movement might discourage the eggs from staying attached to the follicle. The visual that was offered was that of ripe apples hanging at the ends of tree branches sensitive to being shook off.
Rest and injections were the routine before, during and after each IVF cycle.
News of the result of each round of IVF was delayed by 2-3 weeks due to the secondary genetic testing we were undertaking. This meant we were held in suspense as we waited to hear how many embryos survived and were viable at least to proceed towards the embryo freezing phrase. Some news was good, some not. None of the four eggs from Canada survived. All that expense, time and worry—for nothing.
Egg Harvesting Cycle #1, June 8, 2019
The first round of IVF resulted in three embryos. Of those, one was genetically mosaic, meaning that the cells that were tested were not matching each other, and likely meant that the embryo was not viable. One of the other embryos was a female carrier of Fragile X. The third egg did not fertilize successfully.
Egg Harvesting Cycle #2, July 3, 2019
The second round of IVF harvested four eggs but resulted in no live embryos. Sharing the news with Emily, we were heartbroken. We had now spend over $40,000, dozens of injections and pills, and months of effort. Now we had only the thinnest of possibilities of having a baby through traditional means. After a little grieving, we calmed our nerves and committed to figuring out our next step.
Egg Harvesting Cycle #3, July 16, 2019
While not our original plan, we scraped together money and got a generous loan from Emily’s mom to cover one final round of IVF. On my birthday (July 26), I returned again with Emily to SRM and we underwent the final egg harvest. After the quick procedure we learned that two eggs were successfully harvested and fertilized.
Three weeks later I got a call from Dr. Dudley.
“Joel, I have the test results from the latest round.”
“Great! How did it go?, I asked.
“We have one embryo that made it through to insemination and survived. It is typical.”
This was amazing news! When counting our first round, we now had two embryos! I couldn’t wait to share the news with Emily.
She was on a hiking trip with Luna and the plan was for me to climb up into the Alpine Lakes Wilderness and spend the last night with her before descending together the next morning. I couldn’t contain my excitement as I ascended. The phrase that kept repeating in my mind was “typical”. Normally this would not have been a compliment, but in this instance the phrase meant the embryo was healthy, and a second opportunity for us to have a baby.
I arrived at Melakwa Lake just before dark and shared the wonderful news.
We have one more embryo—this one is ‘typical’!”
Emily was excited for the news and to see me, but was also emotional knowing the toll she paid over the past few years as we’ve navigated this process.
IVF Bills
The costs throughout the entire experience were extraordinary. We luckily had a friends and family discount thanks to a referral from a trusted friend and SRM nurse, but that only blunted part of the costs. Each round of IVF ran us over $10,000, plus medications (there were lots), genetic testing by a third-party provider, blood work, cryogenic shipping costs for the eggs from Canada, and on and on and on. In total we probably spent about $60,000, but honestly I have no idea what the true figure is. Almost nothing was covered by health insurance and we were below the threshold to qualify for a Federal tax credit for medical expenses, so we relied on savings and bonuses to cover the costs. Luckily Emily had saved thousands to cover the expenses, and I contributed where I could with each cycle and to cover the required medications.
During this time our family grew by one fur baby. Welcome Maple!
The embryos stayed frozen over the next two years as Emily and I bought another house, adopted our puppy Maple and got engaged and married. Our wedding ceremony destination was a fire lookout adjacent to Crystal Mountain and in the shadow of the majestic Mt. Rainier. Friends Leon and Jill and their son Arthur plus Emily’s mom served as officiants. Using a tripod and a timer, I served as the day’s photographer, videographer and groom. It was perfect!
Wedding proposal at Aasgard Pass, Leavenworth, WA
Emily and I were married at Suntop Lookout, a beloved destination in the shadow of Mt. Rainier.
Just two days after saying “I do!”, Emily and I returned to SRM for our first attempt at getting pregnant. We had the one “typical” embryo implanted, and then Emily started daily injections of Progesterone for over sixty days, plus other medications and screenings to help the microscopic embryo take. We had just two chances at this so we tried our best to adhere to the doctor’s orders and played it safe.
An image of the embryo taken just prior to implantation.
Two weeks after the implantation Emily did another blood test and we got some amazing news.
“You’re pregnant!” shared Dr. Dudley.
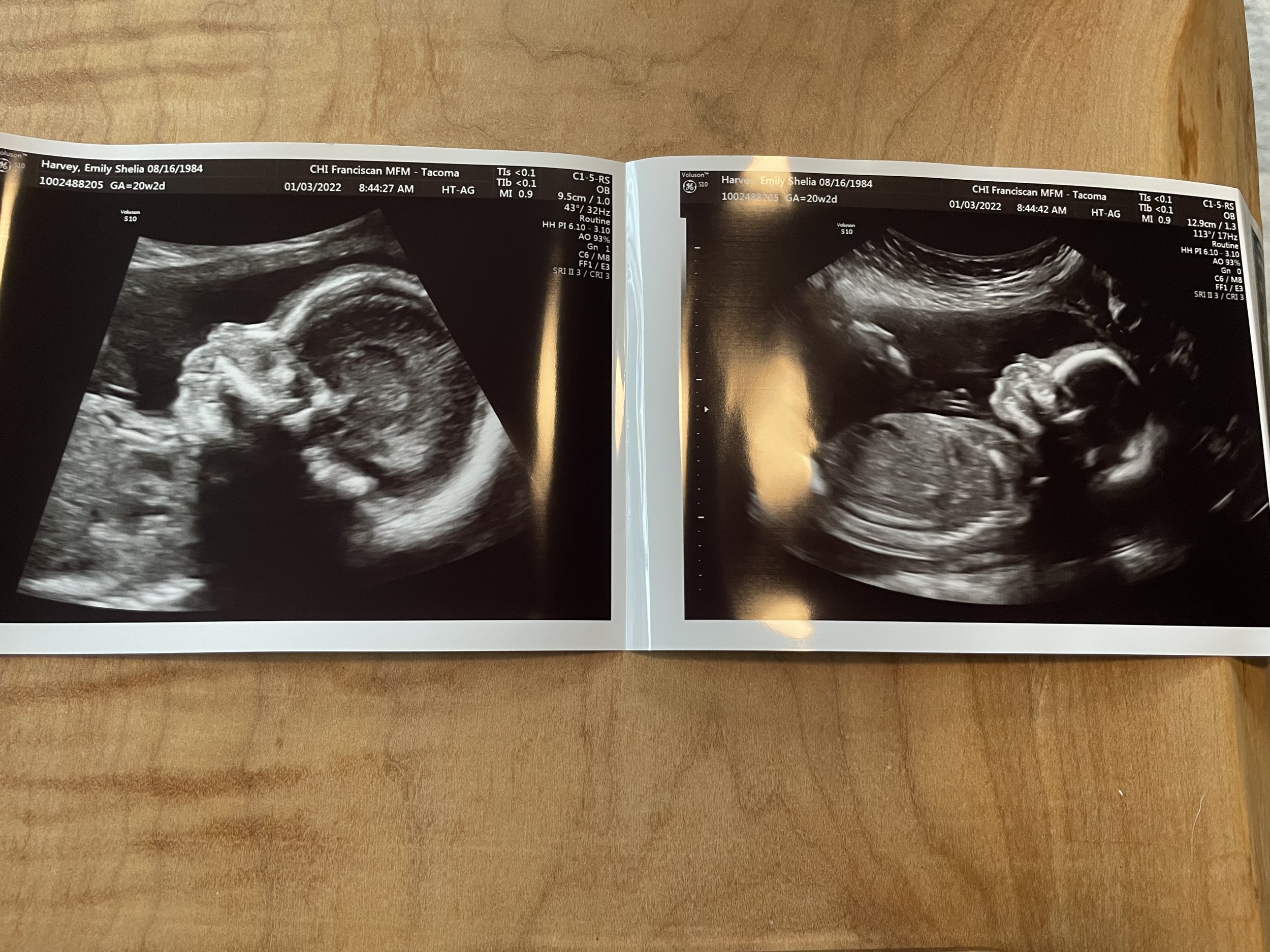
Amazing! After years of effort and countless restless nights we finally had at least a chance at a baby. Emily continued to rest, do her injections and take her medications and prenatal vitamins without complaints despite the burden. Each subsequent screening at SRM had more encouraging news. We were on track and at 13 weeks we “graduated” from the fertility center and transitioned to care at St. Joseph’s Midwifery. Everything looked to be developing well. Just two days after the New Year, we had the anatomy scan and the ultrasound returned positive news.
The baby looked healthy and was developing at a solid pace.
Rest up little baby, rest up.
Emily on February 2, 2022, her last flight before she lost her medical and reverted to solely teaching in the simulator.
Grow Baby, Grow
We also took weekly photos to document the pregnancy. Emily would pose in our bedroom at our old house holding a chalkboard marked with the weeks. She even volunteered to take on extra shifts each month to pad her savings in advance of the planning and unpaid maternity leave. Luckily, after getting over some initial shocks due to all the supplemental hormones early in her pregnancy, Emily had few other side effects during the first and second trimesters.
The third? That was something else.
In the third trimester she had intense insomnia and frequent bouts of indigestion coupled with restless leg syndrome. We threw every medical and folk remedy at these ills to little effect—Tums, Calm magnesium supplement, pillows, buckwheat heating pads, Pepcid AC and many others, but the discomfort persisted. Nights would go by and it would take Emily 6-8 hours to fall asleep. I would sneak the dogs out the next morning for breakfast and a walk just as Emily was finally getting some sleep.
During the third trimester, we also bought and moved into a new home while renovating and renting our previous house. It was hectic and exhausting, but probably good training for having a baby.
With a month to go, Emily decided that she had to start her maternity leave. Her job as a Horizon Air simulator instructor required her to be locked in a moving Q400 sim for hours at a time as she instructed new pilots and captain upgrades on how to master the aircraft. It was physical and the heartburn was unrelenting as the large structure sat atop hydraulic pistons that tilted and rocked the sim as the pilot navigating the aircraft. Yup, exactly what you don’t want to experience when you’re struggling with indigestion.
Unlike almost all other WA state workers, Emily did not qualify for our Paid Family and Medical Leave Program because her career in the airline industry was overseen by Federal law which offers no such benefit (huge fail Congress!). Instead, Emily would take unpaid time off after exhausting a small amount of short-term disability for her maternity leave. Luckily, I have family health insurance to cover the lapse that she may encounter after the baby is here, plus we saved to ensure we could financially afford a loss of income. Our plan was for me to take leave from my work when the baby arrives for four weeks. I would then go back to work through to the end of October when I would start my three-month parental leave. Emily would then transition back to work in early November while I stayed home and cared for the baby through until January 2023.
I’m certain there will be hardships ahead—every parent we’ve spoken to has warned us of lost sleep and exhaustion, but we are ready. After running this gauntlet for years, my hope is we’ve developed the skills to deal with setbacks and surprises. I’m not a religious man but I do believe in letting go to a greater power…trusting that we’ll all just figure it out.
UPDATE: May 24, 2021, 1:32PM PST - “It’s a BOY!”
Special Thanks to Miranda Jade Photography
Introducing Jack Ballezza! Born Tuesday, May 24th at 1:30PM this chunky monkey rang the scale at 9lb 5oz and 21 inches long following 37 hours of labor by the brave and determined Emily Harvey. While the original plan was a natural home birth, after 16 hours laboring in our bedroom with our midwife and doula, we knew we’d need even more help and medication to welcome the baby.
We headed to St. Joseph Hospital around 7PM on Monday, and as luck may have it our original midwife Claudia was on duty. She ordered painkillers and cared for us in triage before we were admitted. After a few hours we finally landed a room which also meant Emily could get relief using an epidural. By 11PM or so on Monday, Emily finally had her first relief from the contractions in almost 24 hours.
Emily pushed on and off using a squat bar attachment for her hospital bed and all her might. Despite pushing late Monday night and into the next morning, the baby wouldn’t descend.
At noon on Tuesday we consulted with the OBGYN, midwife and nursing staff. After another cervical check we discovered that the baby was occipital transverse (head sideways in birth canal). This was bad news— especially when combined with Emily’s narrow pubic arch. We decided the vacuum method was too unsafe so we opted for a c-section.
By 1:30PM, the baby was here!
I was filming and watching from right next to Emily as the surgery was done on the other side of the drape. I grasped Emily’s hand as she shook from trauma and nerves. She was particularly brave as they wrestled the baby out of the 8-inch incision made to her abdomen and the anesthesiologist cautioned to anticipate “heavy pressure.”
“It’s a boy!” Emily called out when they passed Jack over the drape to her, all while a geiser of urine—his first open air pee—arced over the operating table. Within minutes we were all back together in our hospital room and spent the next two days caring for Jack and changing his numerous diapers. We were blessed: one embryo attempt, one pregnancy and one healthy baby to term.
We got here thanks to four rounds of IVF, genetic testing, daily hormone shots, worry and waiting, love and good old fashion determination. After three years of effort, we had a baby! If anyone wants to know more about the IVF experience, please reach out.
Baby & Maternity Photos
Special Thanks to Miranda Jade Photography